A Patient-Centered Approach
A Patient-Centered Approach
Putting Patients at the Center of Care
Exploring the Quintuple Aim and Value‑Based Care
Performance measures have become increasingly important for healthcare transformation. Improving the patient experience is a key objective and a component of the Agency for Healthcare Research and Quality's Quintuple Aim. This initiative seeks to put patients at the center of care with 5 common goals1,2:






Better Health refers to both healthy people and, at a broader level, healthy communities. This aim requires the implementation of proven interventions that address behavioral, social, and environmental determinants of health.1
Affordable Care involves reducing the cost of quality healthcare for everyone: individuals, families, employers, and the government.1
Provider Satisfaction aims to improve the work life of healthcare providers so they are better able to care for their patients.2
Health Equity focuses on providing every person with an equal opportunity to achieve their full health potential.2
Better Care means improving the overall quality of care by making healthcare more patient-centric, reliable, safe, and accessible.1
Value-based programs have been introduced to incentivize healthcare providers to deliver quality care at a lower cost. These value-based models are intended to replace fee-for-service payment systems.3
To learn more about the Quintuple Aim and strategies for quality patient care, go to the Agency for Healthcare Research and Quality website. For more information on value-based programs, go to the Centers for Medicare & Medicaid Services website.
The All For One Purpose
Engaging with the patient and their support system by sharing resources and communicating effectively can help enhance the patient experience—a critical aspect of nuclear cardiology care. Astellas offers educational patient and provider resources that span the cardiac testing journey, promoting collaboration and communication, effective prevention and treatment practices, and the safe delivery of care. Beyond this, the tools and information you’ll find on All For One Cardiovascular can help you develop a shared language and understanding of care.
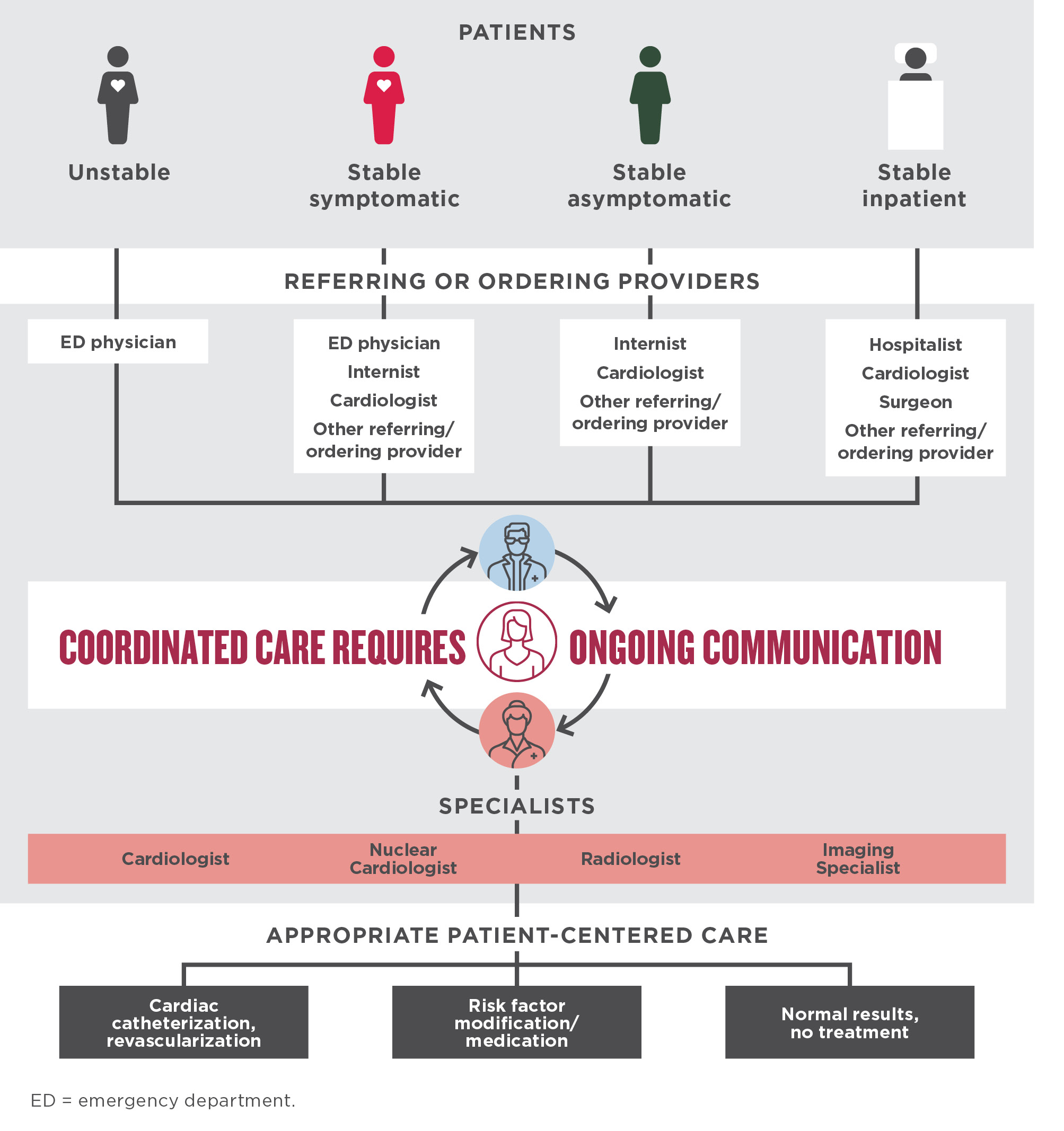
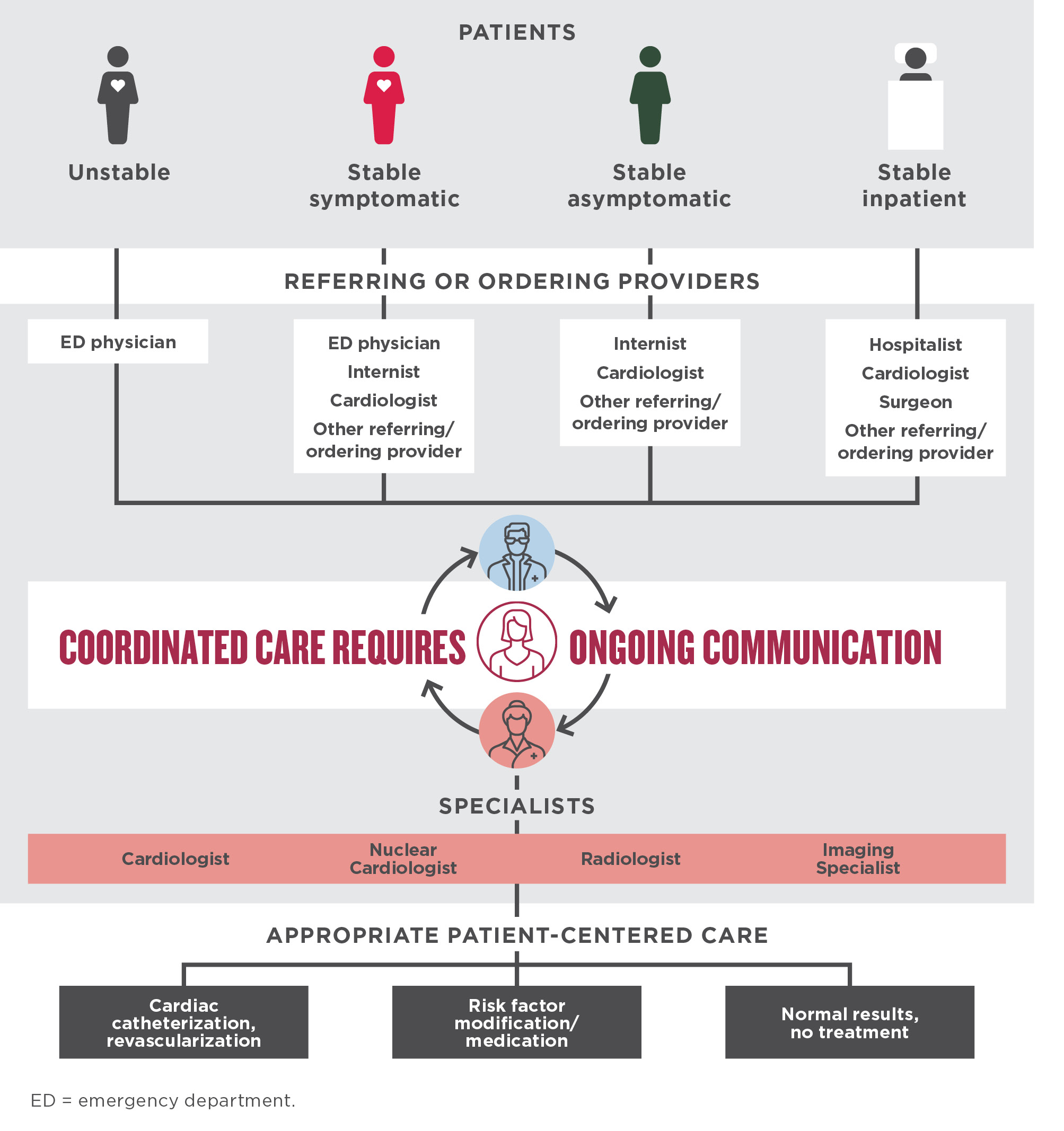
ACCF/AHA Recommendations for Establishing a Collaborative Culture
Regardless of patient presentation, effective communication between specialists, referring and ordering providers, and the patient is crucial for making informed decisions about patient cardiac risk and management plans.5 For each of the patient scenarios highlighted below, ongoing communication is necessary for coordinating patient-centered care.5-7
ACCF = American College of Cardiology Foundation; AHA = American Heart Association.
Electronic Information-Sharing and Communication
Electronic medical records (EMRs) can help facilitate communication and collaboration between referring and ordering providers and imaging specialists by providing access to information about the patient history, lab results, risk assessment, diagnostic results, and treatment plan, according to an article in the Canadian Family Physician. Multidisciplinary team members can review the EMR and add information and notes to help improve patient care across the care continuum.8
ASNC's Patient-First Imaging
The American Society of Nuclear Cardiology (ASNC) supports a patient-first approach to multimodality imaging for the assessment of cardiovascular disease. Selecting the right test for the right patient at the right time is the focus.9
The patient-first strategy includes:
- Optimal test selection
- Optimal equipment
- Optimal image acquisition and processing
- Optimal interpretation and reporting
Diagnostic testing strategies should be in compliance with appropriate use criteria. When multiple testing modalities are considered appropriate, local expertise and availability of quality equipment factor into the imaging decision.
ASNC's patient-first strategy helps ensure patients have access to the appropriate cardiovascular imaging test that is optimal for their care.
ASNC Guidelines for Image Interpretation
Accurate image interpretation is important to clinical decision-making. For cardiovascular service line (CVSL) managers and team members who may be new to image interpretation, ASNC recommends systematic interpretation of SPECT MPI images that may include10:
- Raw-image evaluation in cine mode to identify potential artifact sources and extracardiac tracer activity
- Identification of location, size, severity, and reversibility of perfusion defects
- Assessment of cardiac chamber sizes and pulmonary uptake
- Incorporation of quantitative perfusion analysis
- Consideration of functional data from gated images
- Consideration of clinical data that may influence interpretation
These factors should be considered prior to generating the final report.
ACCF Guidelines for Structured Reporting
The final report is an essential component of any cardiovascular imaging test.11 Imaging results should provide critical information to the referring provider in a comprehensive and clinically relevant manner. Structured reporting is central to effectively communicating the imaging results to referring or ordering providers.12
Structured reporting should strike a balance between consistency and flexibility, completeness and conciseness, required elements and optional elements, and the universal and proprietary. According to the ACCF health policy statement, along with guidance from multiple other organizations, the key principles of structured reporting are shown below.11
Explore these sample reporting templates in the ASNC guidelines publication on standardized reporting.
In the case of critical test results that are significantly outside the normal range and potentially life-threatening, the National Patient Safety Goals recommends that imaging labs implement procedures for timely reporting so patients can receive prompt treatment. The procedures should include a definition of “critical results,” establish an acceptable timeframe for reporting, and determine who should report and who should receive the critical results.14

Helping to Improve Quality of Patient Care
Ongoing assessment of laboratory practices is an integral part of maintaining quality performance. According to the Intersocietal Accreditation Commission (IAC), quality improvement in the nuclear lab should emphasize accuracy and efficiency, safety for patients and staff, and the patient experience. These initiatives can help15:
- Reduce the need for repeated studies due to poor image quality
- Increase diagnostic accuracy
- Reduce radiation exposure
- Improve the patient experience




As illustrated here, quality improvement is a continual process of assessing performance and identifying opportunities for change.15
The patient experience is a core measure of performance and quality improvement.15 According to the IAC, other potential areas for evaluation include imaging quality and safety, test appropriateness, interpretation quality, and timeliness of reporting.16
The IAC offers a tool for assessing quality improvement activities and meeting the quality measures required by the IAC Standards.
aAdapted from: Farrell MB, Abreu SH. A practical guide to quality improvement in nuclear medicine. J Nucl Med Technol 2012;40(4):211-9.
References+
1. Agency for Healthcare Research and Quality. Introduction to the National Quality Strategy. https://archive.ahrq.gov/workingforquality/nqs/toolkits/nqs-intro.pdf. Accessed 12-01-2023.
2. Agency for Healthcare Research and Quality. AHRQ evidence-based Care Transformation Support (ACTS). https://digital.ahrq.gov/acts. Accessed 12-01-2023.
3. Centers for Medicare & Medicaid Services. What are the value-based programs? (09-06-2023). https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/value-based-programs/value-based-programs.html. Accessed 12-01-2023.
4. Boland GW, Glenn L, Goldberg-Stein S, et al. Report of the ACR’s economics committee on value-based payment models. J Am Coll Radiol 2017;14(1):6-14.
5. Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: executive summary. J Am Coll Cardiol 2012;60(24):e44-164. Erratum in: J Am Coll Cardiol 2014;63(15):1588-90.
6. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes. Circulation 2014;130(25):e344-426. Erratum: Circulation 2014;130(25):e433-4.
7. Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol 2014;64(22):e77-137.
8. Manca DP. Do electronic medical records improve quality of care? Can Fam Physician 2015;61(10):846-7.
9. Thompson RC, Calnon DA, Polk DM, et al. ASNC statements of principles on the issue of multimodality imaging. J Nucl Cardiol 2021;28(5):2456-2457.
10. Dorbala S, Ananthasubramaniam K, Armstrong IS, et al. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol 2018;25(5):1784-846.
11. Douglas PS, Hendel RC, Cummings JE, et al. ACCF/ACR/AHA/ASE/ASNC/HRS/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR 2008 health policy statement on structured reporting in cardiovascular imaging. J Am Coll Cardiol 2009;53(1):76-90. Erratum in: J Am Coll Cardiol 2009;53(16):1473.
12. Douglas PS, Chen J, Gillam L, et al. Achieving quality in cardiovascular imaging II. JACC Cardiovasc Imag 2009;2(2):231-40.
13. Tilkemeier PL, Bourque J, Doukkey R, Sanghani R, Weinberg RL. ASNC imaging guidelines for nuclear cardiology procedures: standardized reporting of nuclear cardiology procedures. J Nucl Cardiol 2017;24(6):2064-128.
14. The Joint Commission. National Patient Safety Goals® effective July 2023 for the laboratory program (03-29-2023). https://www.jointcommission.org/-/media/tjc/documents/standards/national-patient-safety-goals/2023/npsg_chapter_lab_jul2023.pdf. Accessed 06-09-2023.
15. Farrell MB, Abreu SH. A practical guide to quality improvement in nuclear medicine. J Nucl Med Technol 2012;40(4):211-9.
16. Intersocietal Accreditation Commission. The IAC standards and guidelines for nuclear/PET accreditation (06-23-2023). https://intersocietal.org/wp-content/uploads/2023/06/IACNuclearPETStandards2023.pdf. Accessed 06-23-2023.